Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): Emerging Insights and Cardiovascular Connections
Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): Emerging Insights and Cardiovascular Connections
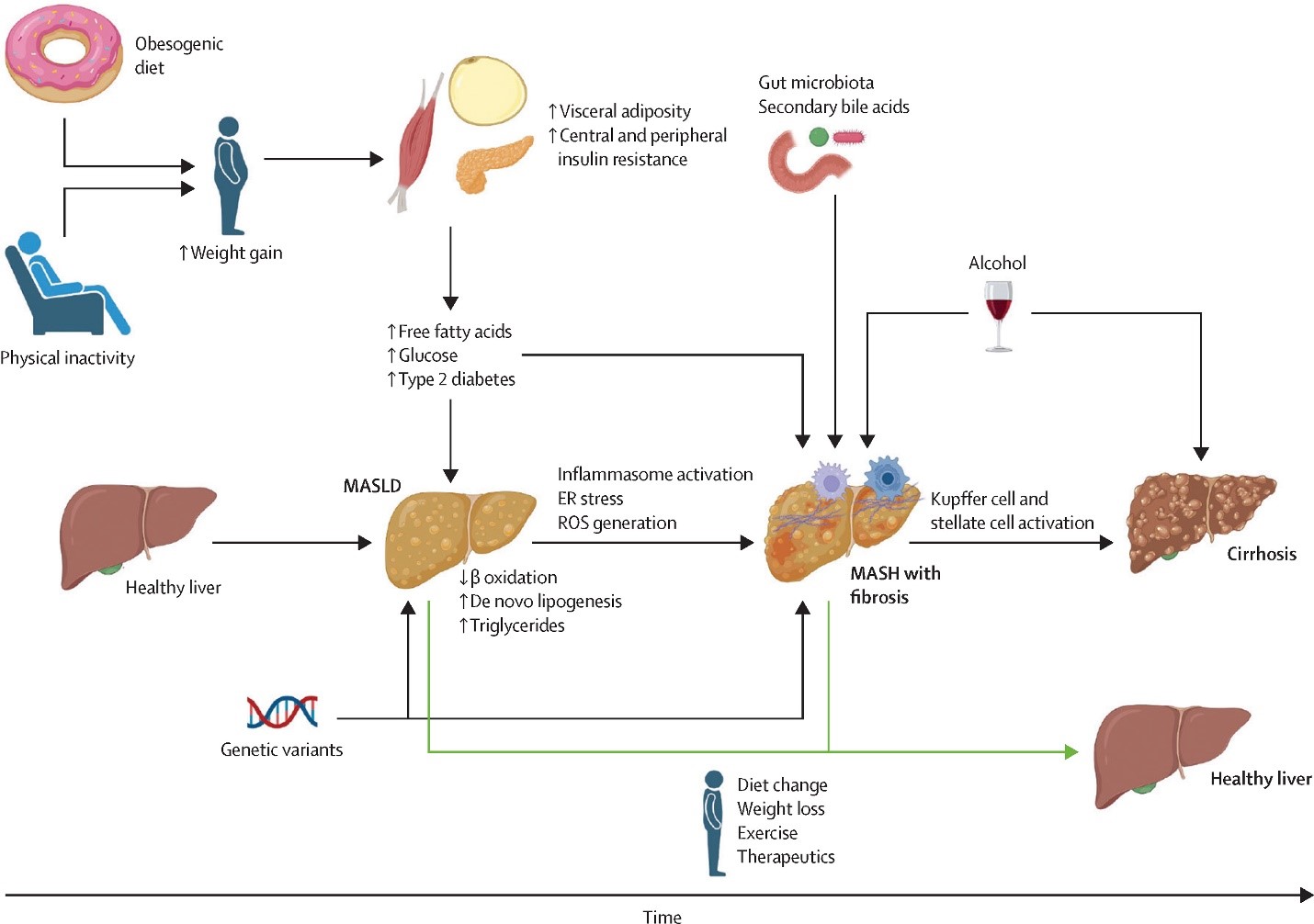
Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), formerly termed non-alcoholic fatty liver disease (NAFLD), has emerged as a critical player in cardiovascular disease (CVD) pathogenesis. Characterized by hepatic fat accumulation alongside metabolic dysregulation—insulin resistance, obesity, or dyslipidemia—MASLD is now recognized as both a precursor and amplifier of systemic inflammation and endothelial dysfunction. Recent studies underscore its bidirectional relationship with CVD; individuals with MASLD exhibit a 2- to 3-fold increased risk of atherosclerosis, arrhythmias, and heart failure, independent of traditional risk factors. A groundbreaking 2023 Journal of Hepatology study identified MASLD-driven alterations in gut-derived metabolites (e.g., trimethylamine N-oxide, TMAO) as key mediators of vascular inflammation, offering novel therapeutic targets. Additionally, advances in non-invasive diagnostics, such as MRI-based proton density fat fraction (MRI-PDFF) and elastography, are refining risk stratification and enabling early intervention.
Intriguingly, 2024 research in Nature Reviews Gastroenterology highlights mitochondrial dysfunction in hepatocytes as a unifying mechanism linking MASLD to cardiac remodeling. Interventions targeting mitochondrial dynamics—such as PPAR-α agonists and lifestyle modifications emphasizing aerobic exercise—show promise in reducing hepatic and cardiovascular fibrosis. Furthermore, a 2024 Clinical Gastroenterology and Hepatology trial demonstrated that combining GLP-1 receptor agonists with Mediterranean-style diets synergistically improves hepatic steatosis and coronary microvascular function. These findings position MASLD not merely as a hepatic disorder but as a multisystem condition demanding integrated cardiometabolic care—a paradigm central to our center’s preventive strategies.

comment